Saturday, September 21, 2013
Only the Flu?
In the past 2 weeks I have heard of THREE different children dying because of a missed Type 1 Diabetes diagnosis. Two of those children were infants, one 8 month old and one 10 month old. These children's parents were told that their child's symptoms were "the flu" or some other similar malady. There is so much awareness and training for Type 2 diabetes, which is by far more common than Type 1 and comprises about 85-90% of people with diabetes. But type 1 has far more serious consequences if not taken care of immediately when symptoms present. With cold and flu season soon upon us I would like to share with you the common symptoms of type 1 diabetes that often get written off as something non-serious.
1. Frequent urination
2. Excessive thirst
3. Fruity or winelike smelling breath (can also sometimes smell like acetone)
4. Excessive hunger
5. Blurred vision
6. Fatigue/lethargy
7. Vomiting
8. Labored breathing or wheezing
9. Sudden unexplained weight loss
Most of these symptoms alone are not too worrisome on their own, and most general practitioners are not trained in identifying and treated type 1 diabetes. If your child is experiencing these symptoms and you take them to the dr, ask for them to do a fingerstick to check blood sugar and/or a urine dipstick test to check for sugar or ketones in the urine. IF these tests are done and the dr thinks it might be diabetes, go to the ER or hospital. As I previously stated, most dr's are trained in Type 2 Diabetes which doesn't usually require emergency care at onset because the pancreas is still producing insulin it just doesn't use it efficiently. With type 1 diabetes the pancreas does not produce insulin (or not enough) and the body will essentially starve to death because it cannot use the food for fuel and will start breaking down fat stores to function. The byproduct of the body burning fat for fuel are called ketones and they can cause the blood to become acidic (ketoacidosis) Organ damage or failure can result if diabetes is left untreated, especially the kidneys.
Again, I am not sharing any of this to scare anyone, but to encourage parents to ask for a simple test if the dr is not sure if your child's symptoms are the flu. Angelina had a cold the week of her diagnosis, she started using the restroom a lot, drinking a lot and complaining of her eyes being blurry. I thought she was dehydrated from being sick. It was 3 days from when that first symptom occurred until I took her to the dr, and I took her because the cold was getting worse instead of better (it ended up being pneumonia), not because of the other symptoms. She spent 4 days in the hospital getting her blood sugar down to normal levels and was in mild diabetic ketoacidosis. She had lost about 5-7 lbs in 2 weeks, and I wrote it off as a growth spurt because she always gets taller before she gains weight.
I have talked to numerous other parent's in the Type 1 Diabetes community and most of their stories are similar to ours - they thought their child had a UTI, or was dehydrated, or had the flu. They didn't have diabetes in their family so they never even considered that it could be that. Diabetes isn't only a familial disease. Only 10-15% of people with type 1 diabetes have a relative with diabetes.
If you would like more information about Type 1 Diabetes you can go the American Diabetes Association (ADA) webpage. The Juvenile Diabetes Research Foundation (JDRF) also has some good information. Or, feel free to email me at: Type1DMom@outlook.com and I will try to help point you in the right direction.
We need to get the word out so kids can stop dying because of a lack of education and awareness. Type 1 diabetes is a very treatable disease. It's not easy, by any means. But it is treatable, and people with diabetes can and will go on to lead long and fulfilling lives with proper education and treatment.
Friday, August 30, 2013
‘Round Here
Related articles
- First Day of the 5th Grade (chasinglows.wordpress.com)
- Random Foods that Make My Blood Sugar Act a Fool! (diabetesdaily.com)
Friday, August 23, 2013
Somebody had a birthday!

Here's how the day went: Went to the school at lunch time only to find out there will actually be two aides who will be taking turns helping Ang in the clinic. Normally, the more the merrier, but with Ang and her specific case I do not like not having just ONE person who is in charge of things at the school. I think having 2 people will likely lead to some confusion, and possibly a delay in treatment if they have to scramble to figure out who to call to come to her in an emergency since neither of the aides full time job is in the clinic. They are both aides helping other disabled or special needs kids in their classrooms and are pulled out if/when Ang comes to the office. I'm very frustrated about this situation because IF there is an emergency with her every second counts and precious minutes could be wasted while office staff try to figure out who to call and the amount of time it takes for that person to respond and get there. Both aides are in classrooms literally across the school from where Angelina's classroom is, and the office is halfway between both.
I was able to get the living room and kitchen cleaned in the afternoon after picking up her cake (which was beautifully done and she loved it!). David got home around 4:30, so only 30 minutes later than planned, but he bought her a rose bouquet on his way home so I think that makes up for it. She decided she wanted to order pizza in for dinner and we ate around 5:45pm. Pizza is a particularly hard food to dose insulin for because of the very high fat content it has a nasty habit of being slow to digest which means that it usually really effects blood sugars a while after her insulin has already done it's job. She decided to only eat 1 piece though so that definitely helped. She loved her presents, most of them she already knew about or helped pick out, so I did have a couple surprises in there, including the movie "Epic" which I picked up when I got her cake. She got Minecraft (game) on her phone and got pretty absorbed in that most of the night. I asked her what she wanted to do and did we want to do some family time but she was content playing her game so we just all had a low key kind of night. After cupcakes we put on her new movie and when it was over it was time for bed. There was no fighting/bickering. The only thing that even stands out is she insisted on lighting the candles on her cake and kept holding the match/candle downward and burning her finger and getting wax everywhere so David started to help by lighting candles on the other side and she had a mini-fit about it but recovered quickly and was happy again.
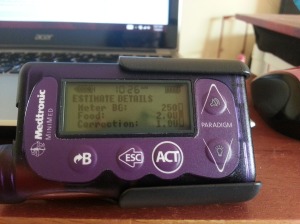
Now for the technical stuff about how things went with her diabetes: I checked her blood sugar shortly after David got home and she was around 250, her target range being 100-150, so we did a correction to get her closer to target before we even ordered the pizza. By the time we got the pizza and went to eat she was around 175, which is not a bad starting point. At 2 hours post-pizza she was 213 and we went ahead and did cupcakes. She got insulin for 1 cupcake and then a separate dose with her 2nd cupcake and a glass of milk. The second dose we did as a "dual wave" which means she got a small amount up front (since she already had some insulin going to cover the first cupcake and what was left of the pizza) and the rest of her dose slowly over 3 hours to help combat the likely spike from fat content. That was around 8:00. I checked her at 11:30 again, 30 minutes after the insulin dose was done and she was 201 with a small amount of insulin that was still working. This morning she woke up at 162, which is pretty close to her target range and is a perfectly acceptable number to me. Here is how a type 1 diabetic celebrates their birthday: The same as anyone else - with CAKE!!! And a side of glucose meter and insulin.

Related articles
- She Can't Eat That...She Has Diabetes! (chasinglows.wordpress.com)
- First Day of the 5th Grade (chasinglows.wordpress.com)
- Differentiating between Diabetes Mellitus Type 1 and Type 2 (epicahealth.com)
Wednesday, August 21, 2013
First Day of the 5th Grade
So, that stress I knew about yesterday. The principal seemed very nice and very informed. She said she had t1 students at her previous school and seemed to know quite a lot for someone who wouldn't have been involved with day to day care. Unfortunately she won't be the person involved with Angelina's day to day care either. The new office manager seems very stressed out, but enthusiastic, so I think she will be an ally. I can't imagine it's easy being the new person in charge of everything on the first day of school. So, the aide. Well, I was hoping for the best because when I spoke with DN (district nurse) yesterday she said that even though the new aide wasn't going to be in the clinic all day, that she would be available to come if Ang came in. She told me that the aide had been assisting another t1 student (with a pump) at a different school for the past few years, and that student had graduated to middle school this year, which is why she was placed at our school. So, that sounded promising. Or at least not terrible, since we lost the fabulous nurse we had last year. And then, this morning when I went in to have a brief meeting with everyone the new aide was not there and I was informed that she doesn't start until 8:30.
School starts at 8:35, Ang gets there around 8:20 if she rides the bus. I tell myself it's not a big deal, because she will have just eaten breakfast before leaving the house and I would know what her BG is and she normally wouldn't get checked between breakfast and lunch anyway unless she didn't feel good. So, I was asked to come back at lunch to teach them how to use Ang's pump. This is something different because last year after diagnosis she was still on shots. She just started pumping in mid-July. The DN and I agreed to meet at the school at 11:45, since Ang's lunch is at 12 and that would give us a few minutes to get introductions out of the way and things settled before Ang came in for her check. Well... I get there at 11:45 and neither the DN or the aide are in the office. So I stand around waiting and writing some info in the packet of papers that I brought with me about how to use the pump. A lady walks in the office and sees that one of the papers has a glucose meter picture on it. She asks if I'm there about diabetes. I said I was a parent and that yes, my daughter had diabetes. I asked if she was the new health tech. She said no, but that the aide had sent her to find out what time she was supposed to be in the office for Angelina's lunch, because she didn't know what time her lunch was. All I can say is that I'm glad it wasn't last year, because her lunch was at 11:40 and she would have missed it. Did I mention that AM Kindergarten is in session until 11:55?
Anyway, a few minutes later this lady walks into the office eating something that smelled like nuts out of a ziploc baggie, kind of looks at me and says, "Are you the mom of the diabetic?" I said "I'm Angelina's mom." She said "Oh, hi, I'm L. I'm going to be the one checking your daughter's blood sugars." Right off the bat this sends off TONS of red flags. She then goes on to tell me she's SO hungry because she didn't get a break and didn't get to eat breakfast and that was what she was eating. I asked if it had nuts in it and she said it's cereal. I said "Oh, that's good. It smelled like nuts and Angelina has a severe nut allergy." She then decided that she needed her water and she said she was going back to the classroom since no one else was there yet. While she was gone the nurse finally showed up and heads into the clinic (which is really just a little 10X10 room with a bunch of filing cabinets, a counter and some cupboards and a sick bed in it). I asked about the aide because the name she had given me was different than what the nurse had told me yesterday. She then told me there was a last minute change and this aide was NOT the person who had been overseeing the other kid with diabetes at the other school. Joy. Angelina is a few seconds behind her and starts unpacking her lunch to add up her carbs. Meanwhile, the aide is not back yet and Ang already figured up her carbs and is ready to go. The aide finally shows up (really she was gone maybe 5 minutes, but in an emergency those 5 minutes can be critical - just goes to show that either the classroom is clear across campus, or she wasn't in a hurry) and Ang gets out her meter and checks herself and pulls out her pump and starts putting in her carbs, etc. I was just like "Whoa! Hold on! We have to teach them how to use your pump because they are going to have to know how to do it." Ang was very anxious to go and was getting very frustrated. So, I quickly walked the aide and nurse through the steps to bolus. This was difficult because the aide had left her reading glasses in the classroom and couldn't see the pump screen. So we convinced ANg that she could unhook and go to lunch and the nurse would return her pump to her when we were done.
While the aide was gone getting her glasses the DN told me that we might be getting a different aide/health tech because they are still moving people around and had some new people enroll in the past 2 days that require an aide. Also, the 2 kids in the kindergarten class were requiring more care than originally thought and the current aide wasn't able to easily and quickly get to the clinic if Ang came in during the time that AM kindergarten was in session. That's not even mentioning what would happen if the aide happened to not be in the classroom if Ang needed her. The aide came back with her glasses and I quickly went over walking her through using the bolus wizard and it made me very glad that I had printed out the cheat sheet instructions that we got for pump training. Then we all went over the dr's orders and what to give her for lows, etc. The aide didn't know the difference between fast-acting and slow-acting carbs for low blood sugars which made me super happy that I decided to separate her snacks and label each container with detailed instructions on when/how much to give for certain blood sugar ranges. I had mostly done that for the office staff on the off chance that one of them needed to treat her.
Going over the dr's orders she didn't understand when she was supposed to check for ketones, even though the nurse had just explained that it was for blood sugars over 300. Then we talked about how Angelina had hypo unawareness under the 60-80 range and that last year many lows were found just because she came in to check for her end of the day check, but felt fine. Then we got into the end of the day check. School ends at 2:45. Angelina rides the bus and in the afternoon is the last stop, so she is on the bus for an hour. (I mentioned in a previous post how the sub health tech last year neglected to call me for end of the day lows and allowed her to get on the bus without rechecking her a couple times. This is a big reason behind me pushing for a t1 504 plan this year. ) So the nurse told the aide that Angelina should come in about 2:40 to check her BG. The aide just looked at her and said "I leave at 2:30, can she come in at 2:25?" The nurse agreed that was fine. Of course I interjected with that was fine as long as her BG was fine, but if she was low she needed to be treated adn rechecked. The aide says "Well, I can just recheck her before I leave." Which, you know, is FIVE minutes later and not nearly enough time for a BG to come up, and that's if she were even able to have checked and eaten a snack in that 5 minute period. However, coming in to check sooner may or may not work because a lot can change in 45 minutes, as all t1 parents know. So I just said "She can come in at 2:20. If she's low, treat her and call me and I will come up to get her. I don't want her to ride the bus if she's possibly low anyway." It really sounded like the aide was just going to give her a juice box and leave her there to her own devices. Fortunately we have not experienced it first hand, but I know it's not uncommon for stubborn lows to not come up right away. Or to come up some and then fall within a short amount of time again - which would likely be right in the middle of her bus ride. I don't WANT to have to pick her up every time she has a low. 1. because for some weird reason she likes riding the bus. 2. because in most cases her BG WILL come up and stay up with a 15 g snack, followed by a BG check to ensure she's over 70 and an additional long-acting snack. But if the aide isn't going to stick around long enough to make sure that her BG came up and stayed that way I'm more comfortable knowing that someone (Me, in this case.) actually is concerned about what is going on with her and making sure she's not crashing hardcore. I feel... cheated.
We had a fabulous nurse last year who was only assigned to her school when she was diagnosed with T1 in March. The nurse was actually an RN, since in CA only RN's can give insulin injections and Angelina was newly diagnosed so not always injecting on her own. Aside from being an RN, the nurse last year also had a dad with t1, and a friend with a pump and she and Angelina shared a love for Hello Kitty. For me, well, she was great about calling me and letting me know what was going on. She also worked at least 8-3 so she was there as long as Angelina was and never said anything about needing to leave if she had to wait a few minutes at the end of the day to treat a low or have me come pick up. (We live across town from the school, it's about a 10 min drive). I know it's not fair to whine about how much this new arrangement sucks compared to last year. But, it sucks. David says I am overreacting and everything will be fine. But I can't help think that things will be fine... until they're not. And I'd rather have all the bases covered BEFORE something happens. I don't want something to happen to Ang before the school/district treat this as seriously as I do. There's a very good reason that I carry an epi-pen and a glucagon kit just about every where with us - insurance. We've never had to use either, thankfully, but that doesn't mean that I get to stop carrying them just because nothing has happened yet. And I would rather have a plan in place and someone who is willing and able to put aside their own agenda to care for her even when it seems like she is doing okay. Because it would only take ONE time of things NOT being okay.
Related articles
- She Can't Eat That...She Has Diabetes! (chasinglows.wordpress.com)
- The Dreaded First Contact (chasinglows.wordpress.com)
- Health: Diabetes can be managed at school as well (state-journal.com)
- Do You Have A Section 504 Plan? If Not, Maybe You Should Get One. (chasinglows.wordpress.com)
- Peanut Allergy Fears | Babble (babble.com)
- We need a change. (dreamsdishesanddiabetes.wordpress.com)
Wednesday, August 14, 2013
The Dreaded First Contact
Hello Ms. Principal,I just wanted to reach out and introduce myself. My name is Jessica and my daughter, Angelina will be a 5th grade GATE student at this year. Angelina was diagnosed with Type 1 Diabetes in March, and I know last year she was the only student at with diabetes. I wanted to see if it would be possible for you and I to meet sometime before classes start next week to discuss Angelina. Last year we worked closely with the district nurse, Ms. Blue Eyes, to set up Angelina's medical plan and I was mostly pleased with the level of care that Angelina received. However, there were some issues that were not covered by her medical plan and I would like to discuss updating her existing 504 plan to include accommodations for her diabetes. I also would like to be allowed to offer training and/or education to any staff members that are willing to learn about Angelina's diabetes and keep an eye on her around campus.In addition to diabetes, Angelina also has ADHD, asthma, anxiety and allergies. The start of the school year is usually very difficult for her and now with the added stress of diabetes I am hoping that you, her teacher and I can work together to ensure as smooth a start to this school year as possible.I will hopefully be up at the school either Monday or Tuesday next week to meet with the nurse and health tech and I would like to introduce myself in person if you have a few moments to spare. In the meantime, if you would like to get in touch with me you can email me, or my telephone number is:XXX-XXX-XXXX, please feel free to call anytime after 9 a.m.Thank you,Jessica <neurotic mom>
Related articles
- Do You Have A Section 504 Plan? If Not, Maybe You Should Get One. (chasinglows.wordpress.com)
- Health: Diabetes can be managed at school as well (state-journal.com)
- Calif. Supreme Court Rules Non-Nurse Trained School Employees Can Administer Insulin (sacramento.cbslocal.com)
- Well, it's about time! (arcillinois.org)
Sunday, August 11, 2013
She Can't Eat That...She Has Diabetes!
As a parent, I will never be as efficient or as exact at dosing Angelina's insulin as her own pancreas was. I can give her insulin, but it won't always be at the right time, or the right dose, and even rarely both. But I can give it to her and I can try my hardest to mimic a functioning pancreas. So, if she wants ice cream, she can have it, just like anyone else. It just means that it comes with a dose of insulin from outside her body. You telling me that my child can't eat something while I am trying to figure out how much insulin to give her just makes my job harder. Maybe I should start telling your pancreas YOU can't eat that. For more information please see points 5, 7 and 12 on the post linked below.
Related articles
- What Parents of Kids With Type 1 Diabetes Want You To Know - A Guide (chasinglows.wordpress.com)
Tuesday, August 6, 2013
Do You Have A Section 504 Plan? If Not, Maybe You Should Get One.
It seems many schools will tell a parent they don't "need" a 504 plan because they can just use the child's DMMP to provide care and accommodations, and will work with the parent to provide additional care that the parent may request. However, the "trap" that many people fall victim to (myself included) is that the DMMP and a verbal agreement with the parent isn't a legally binding document. Which means that the school can tell you they will do things the way you ask, but if someone drops the ball or simply chooses not to follow that agreement, you have little to no legal recourse if something were to go wrong. No one wants to think about the "what if's", especially at school. I think we all want to believe that our child's school has their best interest at heart. And in some cases, it may seem that way. Now, I'm not advocating that everyone go out and demand a 504 plan and then threaten to sue the school the first time they miss a scheduled BG check and your child is fine. I'm just saying that the 504 provides that protection because the school knows that IF they don't follow it to the letter there can be consequences outside of a parent who gets angry. They can attempt to tell an angry parent without a 504 that they're not required to provide accommodations, but they're doing it out of the goodness of their hearts because they care about your child. Warm fuzzy feelings aren't going to protect your child from potential medical negligence though.
When Angelina was diagnosed in March, she was in the middle of spring break, so we had about 10 days before she had to attempt to go back to school. One of the first things I did was contact the school district pupil services director along with the principal at her school through email and let them know that she had been diagnosed with T1 and I wanted to update her existing 504 to include t1 accommodations. I also very firmly stated that she would NOT be returning to school until accommodations were in place. Apparently I was too firm though because it sent everyone into a panic. I got a flustered reply from the pupil services director saying that she would get me in touch with the director of the district nurses to go over a plan. When I spoke with the nursing director she said that for other students with T1 they don't usually do a 504 plan and they just follow the dr's orders and try to make additional accommodations that the parent requests. Here is where I fell into the sense of false security that they would do all this for my daughter out of the goodness of their hearts. I emailed back and forth and played phone tag with the nursing director for a few days getting things in order and by Friday afternoon I had an appointment set up on Monday morning (which was the first day back from Spring Break) with the district nurse who oversees Angelina's school. Angelina and I went to the school that morning and brought all her supplies and doctor's orders. The nurse already had a binder all set up with their logs and info sheets and most of the additional things we had agreed upon that weren't covered on the doctor's orders. I wasn't expecting Angelina to go back to school the next day but they assured me that they were ready for her, and she was enthusiastic about returning so she ended up only missing that 1 day. They placed a new health tech at her school who was an RN.
We live in California and our state law is that only registered nurses can administer injections. Since she was so newly diagnosed she needed help with most of her care still. She did start doing her own injections at school with supervision. However, the "backup" health tech who came when the regular HT was out was only an LPN, which means that he could not administer injections. There were a few days when I would get a call at lunch time that Angelina didn't want to do her own injection and he couldn't do it, could I please come up and give her her insulin. He seemed nice enough and asked a lot of questions about her. Then a few weeks later I was looking over her weekly logs. We had it set up that the paper log they kept of every bg check, every meal, every injection would come home with her on Fridays. Well, I have the most disorganized, forgetful kid so they usually didn't come home on Fridays. I usually only got to see them if I happened to be summoned to the school to do something for her that the HT couldn't do, or if Angelina wasn't cooperating and I remembered to ask for it.
So it was really like every 2 weeks or so that I would get a copy of her log. While reviewing the logs I noticed something pretty alarming - a couple of the days the sub HT was there Angelina had low blood sugars (one day was a 47) and I never got a call. Not only did I not get a call, but there was no record of a recheck and she got sent home on her hour long bus ride like nothing ever happened. Obviously things turned out okay, but it's still scary because what if they hadn't? I never got the chance to speak with her bus driver to relay information about her t1, I don't even know if the bus driver knew about her t1. Not to mention that the bus driver is driving the bus and can't watch Angelina the whole time to make sure she's okay. The other times Angelina experienced lows at the end of the day the regular HT would call me and relay her numbers, what she had to eat or drink to treat it, what her number was after 15 minutes and left it up to me whether Angelina could ride the bus home or if I wanted to come pick her up. After I discovered this lack of notification and follow-up I contacted the district nurse and told her what I had found in the logs. She did say that the sub HT had notified her of Angelina's low. Which is great for record-keeping, not so great for Angelina's safety or my peace of mind. I told myself that he did recheck and just forgot to put it in the log, it was the end of the day. So, I accepted the district nurse's promise to speak with him to make sure he called me if there was a next time. Except a few weeks later I noticed it again on the log, after I had contacted the district nurse. There it was - a 59 - "gave juice, feels ok". No phone call home, no record of a recheck at 15 minutes and she went home on the bus. Since she did end up being okay it was just frustrating. But imagine if that juice and "feeling okay" wasn't enough to bring up her BG. Imagine that she got on the bus and her bg continued to drop and within 30 minutes she "fell asleep" on the bus. Only no one realized it until she didn't get off the bus at her stop and maybe the bus driver didn't notice until she got back to the bus barn. It's scary to think that could happen, but it's not out of the realm of possibility. In that instance though, without a 504 in place I wouldn't have had much legal ground to stand on because "call mom" and "don't send on the bus in case of lows" isn't in the medical plan. That's in the informal verbal agreement that I had with the school. As far as their legal responsibility, the sub HT giving her juice and calling the district nurse to let her know about the low is all he was required to do. In our case, things were okay but I was left with feeling of frustration and worried about if things didn't turn out so well next time. Type 1 diabetes is an unpredictable beast. It doesn't always do what it "should". And I know enough about school red-tape to know that if something "bad" were to happen that the schools' defense would be "We weren't required to notify the parent, and the times that we notified the parent previously were out of the goodness of our hearts." and it's possible that would be the end of that and I would be advised to get a 504 plan that does make them responsible and required to contact me, if that's what the plan says.
A 504 isn't just about keeping the school accountable and helping to prevent accidental gap in care. It also can protect the child from discrimination. There's nothing in my child's medical plan about her being able to attend a class party and have a cupcake. So, if the school doesn't feel up to figuring out her insulin needs and carb counts for a cupcake, without a 504 plan they can say she can't participate becaue of her diabetes. Or, if she has a high BG and needs to use the restroom during standardized testing she can be penalized or get in trouble for getting up and using the restroom. Her medical plan doesn't say anything about allowing her unrestricted restroom access, or extra time to finish a test if her blood sugar is out of range. Or, allowing her to take the test on a different day without penalty. Her medical plan doesn't say that there may be days that she comes in to school late because we were treating a stubborn low BG in the morning. Or maybe we were up half the night treating a low or high bg and she didn't get enough sleep so I let her sleep in for a couple hours and took her in at lunchtime. Normally, all of those would be considered "unexcused" tardies. Which means that they count towards truancy, and too many tardies or absences can lead to legal proceedings against the parents for truancy. Her school district requires a doctor's note for any tardies or absences over 10 in a school year. I don't know about anyone else, but I certainly don't take my child to the doctor every time they experience a low blood sugar.
And Angelina doesn't just have type 1. She also has asthma, allergies and an immune system that likes to catch every illness that goes around and make it worse than it was in the person before. I don't take her to the doctor every single time she has an asthma attack. But I can't send her to school if she can't breathe, right? In 3rd grade she missed a lot of days because she would get a cold that would go straight to her lungs and she would be struggling to breathe for DAYS. She missed most of the month of January 2012 because of this. She would get better for a day so I would send her to school and the next day she would come down with something else that kept her home for several days. I wish I was exaggerating. Her teacher made an offhand comment to me one day about all her absences, I think she thought I was keeping her home just for fun. Especially since she would seem better when I did allow her to go back to school. So, one day she work up with junky lungs, but she said she felt mostly okay. I decided to give her a breathing treatment and send her to school. I dropped her off at 8:30am and went home and waited for the phone to ring. The call to come get her came at 10am. I headed up to the school and went into her classroom to help her collect her things. Her teacher came over and said "She was fine this morning and then all of sudden she just couldn't breathe and started wheezing and coughing! I had no idea!" To which I just responded, "This is why she has missed all of these days lately. This actually isn't that bad, which is why I decided to send her today." Anyway, the point of that is that not every single missed or late day due to a chronic illness requires a visit to the dr, but unless you have a standing document that says that, you are in danger of legal action being taken against you or your child for excessive absences or tardies. In some districts, excessive absences may also equate to the child being forced to repeat a grade, even if they have a passing report card and seem to be grasping the concepts. For additional information on 504 plans and what to pack in your child's school tool kit, please click on the page labeled "Info For School" on the top of this blog. Or just click here.
Related articles
- Diabetes Forecast Magazine Highlights Ways to Keep Kids With Diabetes Safe at School (sys-con.com)
- Managing Your Child's Diabetes at School (ecochildsplay.com)
Saturday, July 27, 2013
What Parents of Kids With Type 1 Diabetes Want You To Know - A Guide
What Parents of Kids with Type 1 Diabetes Want You To Know
A Guide
-
Type 1 Diabetes is an auto-immune disorder. That means that my child's immune system attacked the cells in the pancreas that produce insulin. His/Her pancreas no longer makes insulin. Type 1 diabetes is not caused by eating too much sugar, being overweight, being lazy or any other lifestyle choice. The exact cause is not known at this time.
-
Diet and exercise will not make Type 1 Diabetes go away. The impact diet and exercise has on my child's health is the same as any other person – with or without diabetes. It will keep them healthy, but they will still require supplemental insulin to survive.
-
I am not “drugging” my child by giving them insulin. Insulin is a hormone that is made in the beta cells of the pancreas. Every living person without diabetes produces insulin to help their cells absorb glucose to provide the fuel their cells need. Any food that contains carbohydrates break down into glucose in the body and this is what fuels those cells. In a person with Type 1 diabetes their pancreas does not produce insulin, so they require supplemental insulin through injections or an insulin pump for their body to be able to absorb the glucose for fuel.
-
Without insulin, my child with type 1 diabetes would slowly starve to death, despite eating food. Insulin acts as a “key” to open the cells so they can absorb the glucose in his/her blood. If there is not enough insulin in his/her system those cells will start burning fat for fuel and he/she may develop ketones which are a byproduct of that fat breakdown. Ketones may cause my child's blood to become acidic and result in a condition called diabetic ketoacidosis (DKA) which may result in a coma or death. Excess ketones, left untreated, can cause severe organ damage or even organ failure, especially in the kidneys. The only way to get rid of ketones is to give insulin. Increasing water consumption or IV fluids can aid in flushing out ketones, but will not get rid of them alone, without insulin.
-
I will never be as efficient as a pancreas at determining my child's insulin needs. We do use a formula to decide how much insulin he/she gets throughout the day, but it is a constantly changing formula and it is not always 100% accurate. So many things besides food can effect blood sugar levels, such as exercise, emotions, growth hormones, stress, illness...the list goes on and on. Because of this there will be times, often frequently, that my child's blood sugar may get too high or drop too low.
-
In the case of blood sugar levels that are too low my child is at a very immediate risk of seizure, coma or death if the blood sugar level is not addressed immediately. The quickest way to raise a low blood sugar is through very simple carbohydrate sources like fruit juice, candy, glucose tabs, cake icing, regular soda, or table sugar, just to name a few. Basically anything that is “pure sugar” and does not contain any fat or protein, as these may slow the absorption of the carbohydrates and fail to raise the low blood sugar quickly enough. In the event of a low blood sugar episode these items will not harm my child, and in reality may very well save his/her life. These are “emergency” items and go almost everywhere with us.
-
My child is not on a restricted diet. There is no food that is “off limits” to him/her. My child can eat the foods that he/she has always enjoyed, they just now must be accompanied by insulin to cover the amount of carbohydrates consumed. There is no right or wrong amount of insulin and a greater amount of insulin is not “bad”. Different foods may effect blood sugar levels differently, such as foods that are high in fat and slow digestion.
-
No, I will not take my child in the restroom to give his/her insulin injection. Public restrooms are germy. If you don't want to see him/her get a shot, then look away. Be thankful that you don't require a shot every time you eat something.
-
There is no such thing as a “good” or “bad” blood sugar number. There is only “in range” “high” or “low”. These numbers are used as a guide to assist in the correct dosing of insulin. They are not a “grade” or a judgment of how “bad” my child's type 1 diabetes is. If my child has numbers that are consistently out of range then a dosage adjustment may be needed. This may be due to several different factors, most of which have nothing to do with anything that me or my child are doing “right” or “wrong” in regards to diabetes care.
-
My child is a child first, and there are many times when being a child will come before type 1 diabetes. This doesn't mean that we are neglecting my child's health, it simply means there is more to his/her life than type 1 diabetes. Living with a chronic illness can wreak havoc on a child's emotional health and sometimes being given the chance to just be a kid and not having to worry about diabetes for a few hours is worth it to me, as a parent, as health outcomes are often better when the person is in a better state of mind.
-
This generation of people with diabetes are not likely to see long-term complications from type 1 diabetes. Telling horror stories about your relative who lost their limb or went blind from diabetes is not helpful to my child, or to me. There have been technological advances in the past decade that have made diabetes management much easier and more precise than in previous generations. Managed properly, people living with type 1 diabetes now have a long life ahead of them. In fact, people with diabetes are currently expected to live an average of 10 years longer than people without diabetes due to being more aware of their health status and are more likely to receive prompt medical care than their non-diabetic peers.
-
Type 1 Diabetes is a constant roller coaster that we live with every day. Some days are better than others. It takes a lot of patience and understanding to be a parent of a child with Type 1 Diabetes. I try to reserve my patience for my child. That may mean that I don't have any patience for you right now, which may be why you are reading this guide. Please don't take it personally. My days are hectic, my nights are hectic and chances are I haven't gotten enough sleep lately. I'm sure you mean well, but unless I asked for your advice or opinion, please keep it to yourself. I judge myself quite enough every day, I don't need you to judge me too. I wish I had the time and the energy to educate the entire world about type 1 diabetes, but I don't. I dislike having to constantly correct people's misconceptions, especially when they refuse to listen. My child and I are the ones living this life, unless you or your child also have type 1 diabetes, please don't try to educate me, especially if I haven't asked you to.
Friday, July 26, 2013
High/Low for Week of...??? Hello? Anyone home?
 And really, that was it. We were at the office for maybe an hour and a half. Most of it was just talking (not even really training, but just making sure we had watched all the videos and asking if we had any questions, etc.) and discussing what kind of barrier wipes we should use since she has eczema. How to apply the nifty infusion set IV300 tapes. A brief demonstration of the sure-T infusion sets that our friend was starting out with. We chose the mio sets since they are the canulla type that don't require a separate insertion device (that is the one thing our insurance doesn't pay for). I didn't think Angelina would be willing to try a set that the needle stayed in her with, so the mio won. Sure- T is one of the needle types, which are good if you have teflon allergy or if you end up with a lot of kinked cannulas. Anyway, I got the mio put in my arm as part of the demonstration but our friend's daughter decided she just wanted to do the sure-t set on her brand new Lenny the Lion, who comes complete with areas to do infusion sets!
We left shortly after and headed home. She did complain about the site burning right after we put it in but by the time we were halfway home she said she couldn't even feel it anymore. She did start complaining about the IV3000 later when she was chilling on the sofa, so we ended up taking it off. She was afraid to go to bed with her pump on and asked if she could suspend it for the night. Which prompted a very serious discussion about how the pump needed to stay on because otherwise she wouldn't be getting insulin. I explained it kind of like the pump is now her lantus. Before she would get a shot of lantus and it would last all day until the next shot, but now she's not getting lantus and only getting small amounts of humalog instead through her pump. She was really confused and says "I'm not getting lantus anymore?" I guess she thought the lantus would be in the pump too. We put a tegaderm bandage over the site before she went to bed and she opted to clip her pump onto some PJ bottoms. Everything was fine and in place in the morning and she hasn't worried much about sleeping with her pump since.
However, on Friday I told her she absolutely needed to bathe because, well, I didn't remember the last time I made her take a shower was it had been that long. Was it Monday? Maybe? I just knew it hadn't been since she got her pump hooked up so it had been too long. She was terrified her site was going to come out in the shower though, so I decided to do a site change and let her hop in the shower after taking out her current site. I told her she had to be hooked back up within an hour though. She showered in the record time of 30 minutes, I was amazed. When she got out I popped her new site in, hooked her up, ate dinner, and she was doing great.
I had noticed she was running a little on the high side since we hooked up to the pump, but we had been told to expect that since they usually liked to set her basal rates a little lower to avoid low blood sugar episodes. We had just been doing correction boluses as needed (which was pretty much anytime we checked her blood sugar). We decided to make chocolate covered bananas from a recipe that I saw posted on another D-Mama's blog: Raising Colorado. So we ran out to the store for chocolate chips and bananas at 10pm. Angelina helped by melting the chocolate and kept asking if she could lick the spoon. Then she says "Mom, I'm shaking. I think I might be low." So we stopped our deliciousness making and checked BG: 60. So she slurped down a quick juice and was up to 114 just in time to indulge in some seriously sinful desserts.
When I checked her at 2am her bg was a lovely 165. Of course, in the middle of the night she moved herself out to couch and when I checked on her in the morning she was all wrapped up in her tubing and her site looked like it had pulled out, but her BG was hanging out in the high 100's until later that afternoon so I figured she was fine. She was responding to boluses so we just left it alone. Sunday morning however, she went from 208 at 7:30, to 227 at 11:30, to 335 at 2:30, even after correction at the earlier checks and it wasn't food related since the 335 was right before lunch. So we decided to pull the site since we were on the way to spend the evening at Six Flags. Of course, we were already on our way there when that happened because she had refused to change the site at home before we left just in case the site was fine. We got her hooked up, bolused for lunch and went. At 4:30 she was still hanging around 330, which meant that the site was working, at least, but she wasn't coming down. She was 316 at 6pm and we decided to head home. She was really cranky and it was hot and very busy at the park. WE have season passes and live only an hour away so it wasn't a huge loss. We went on one ride in the two hours we were there.
She did start coming down and was in the mid 200's by the time we got home and 195 at bedtime a few hours later. Then her numbers just kind of bounced around in the 200's and 300's for the next couple of days, even after a slight basal increase on Monday. The correction boluses that we were doing just didn't seem to bring her down much, just slightly prevented her from going up higher. Tuesday she had a couple excursions into the mid 400's. Throughout all of this she was constantly complaining of being hungry and she was just very cranky and difficult to deal with. Thankfully no ketones, so I knew she was getting at least SOME insulin, just very obviously not ENOUGH insulin.
Wednesday she was mostly in the mid 200's again. We did site change, again with no issues. That was the first site that actually made it to 3 days. There was no rash or irritation, although I did hurt her a little taking it out because it was REALLY stuck and I accidentally pulled the canulla out sideways when I was trying to lift the adhesive with a unisolve wipe so I didn't rip her skin off.
We saw her endo yesterday (Thursday, July 25th) and explained that she had just been running way too high so she cranked her basal rates up and adjusted her sensitivity (correction factor) as well. She was actually back in the 100's last night and overnight, and I was really happy. Then she managed to spike a 406 this afternoon, but I think the culprit was a sugary nescafe latte mix that she just had to have a couple hours before. We did a correction and she was down to 250 within an hour and 95 an hour after that (and some play time at the park). I guess we'll have to wait and see if we get nice numbers again tonight. Her 3 overnight checks last night were her first in-range numbers since that 114 last Friday night, that was actually a recovery from a low.
Oh, and there was this:
And really, that was it. We were at the office for maybe an hour and a half. Most of it was just talking (not even really training, but just making sure we had watched all the videos and asking if we had any questions, etc.) and discussing what kind of barrier wipes we should use since she has eczema. How to apply the nifty infusion set IV300 tapes. A brief demonstration of the sure-T infusion sets that our friend was starting out with. We chose the mio sets since they are the canulla type that don't require a separate insertion device (that is the one thing our insurance doesn't pay for). I didn't think Angelina would be willing to try a set that the needle stayed in her with, so the mio won. Sure- T is one of the needle types, which are good if you have teflon allergy or if you end up with a lot of kinked cannulas. Anyway, I got the mio put in my arm as part of the demonstration but our friend's daughter decided she just wanted to do the sure-t set on her brand new Lenny the Lion, who comes complete with areas to do infusion sets!
We left shortly after and headed home. She did complain about the site burning right after we put it in but by the time we were halfway home she said she couldn't even feel it anymore. She did start complaining about the IV3000 later when she was chilling on the sofa, so we ended up taking it off. She was afraid to go to bed with her pump on and asked if she could suspend it for the night. Which prompted a very serious discussion about how the pump needed to stay on because otherwise she wouldn't be getting insulin. I explained it kind of like the pump is now her lantus. Before she would get a shot of lantus and it would last all day until the next shot, but now she's not getting lantus and only getting small amounts of humalog instead through her pump. She was really confused and says "I'm not getting lantus anymore?" I guess she thought the lantus would be in the pump too. We put a tegaderm bandage over the site before she went to bed and she opted to clip her pump onto some PJ bottoms. Everything was fine and in place in the morning and she hasn't worried much about sleeping with her pump since.
However, on Friday I told her she absolutely needed to bathe because, well, I didn't remember the last time I made her take a shower was it had been that long. Was it Monday? Maybe? I just knew it hadn't been since she got her pump hooked up so it had been too long. She was terrified her site was going to come out in the shower though, so I decided to do a site change and let her hop in the shower after taking out her current site. I told her she had to be hooked back up within an hour though. She showered in the record time of 30 minutes, I was amazed. When she got out I popped her new site in, hooked her up, ate dinner, and she was doing great.
I had noticed she was running a little on the high side since we hooked up to the pump, but we had been told to expect that since they usually liked to set her basal rates a little lower to avoid low blood sugar episodes. We had just been doing correction boluses as needed (which was pretty much anytime we checked her blood sugar). We decided to make chocolate covered bananas from a recipe that I saw posted on another D-Mama's blog: Raising Colorado. So we ran out to the store for chocolate chips and bananas at 10pm. Angelina helped by melting the chocolate and kept asking if she could lick the spoon. Then she says "Mom, I'm shaking. I think I might be low." So we stopped our deliciousness making and checked BG: 60. So she slurped down a quick juice and was up to 114 just in time to indulge in some seriously sinful desserts.
When I checked her at 2am her bg was a lovely 165. Of course, in the middle of the night she moved herself out to couch and when I checked on her in the morning she was all wrapped up in her tubing and her site looked like it had pulled out, but her BG was hanging out in the high 100's until later that afternoon so I figured she was fine. She was responding to boluses so we just left it alone. Sunday morning however, she went from 208 at 7:30, to 227 at 11:30, to 335 at 2:30, even after correction at the earlier checks and it wasn't food related since the 335 was right before lunch. So we decided to pull the site since we were on the way to spend the evening at Six Flags. Of course, we were already on our way there when that happened because she had refused to change the site at home before we left just in case the site was fine. We got her hooked up, bolused for lunch and went. At 4:30 she was still hanging around 330, which meant that the site was working, at least, but she wasn't coming down. She was 316 at 6pm and we decided to head home. She was really cranky and it was hot and very busy at the park. WE have season passes and live only an hour away so it wasn't a huge loss. We went on one ride in the two hours we were there.
She did start coming down and was in the mid 200's by the time we got home and 195 at bedtime a few hours later. Then her numbers just kind of bounced around in the 200's and 300's for the next couple of days, even after a slight basal increase on Monday. The correction boluses that we were doing just didn't seem to bring her down much, just slightly prevented her from going up higher. Tuesday she had a couple excursions into the mid 400's. Throughout all of this she was constantly complaining of being hungry and she was just very cranky and difficult to deal with. Thankfully no ketones, so I knew she was getting at least SOME insulin, just very obviously not ENOUGH insulin.
Wednesday she was mostly in the mid 200's again. We did site change, again with no issues. That was the first site that actually made it to 3 days. There was no rash or irritation, although I did hurt her a little taking it out because it was REALLY stuck and I accidentally pulled the canulla out sideways when I was trying to lift the adhesive with a unisolve wipe so I didn't rip her skin off.
We saw her endo yesterday (Thursday, July 25th) and explained that she had just been running way too high so she cranked her basal rates up and adjusted her sensitivity (correction factor) as well. She was actually back in the 100's last night and overnight, and I was really happy. Then she managed to spike a 406 this afternoon, but I think the culprit was a sugary nescafe latte mix that she just had to have a couple hours before. We did a correction and she was down to 250 within an hour and 95 an hour after that (and some play time at the park). I guess we'll have to wait and see if we get nice numbers again tonight. Her 3 overnight checks last night were her first in-range numbers since that 114 last Friday night, that was actually a recovery from a low.
Oh, and there was this:
 One of the things that was the most frustrating is I just felt like we were on our own. I had gotten the impression that we were supposed to contact our pump trainer for adjustments but every time I reached out it seemed like she didn't return my calls, or if she did she didn't really DO anything. It didn't even occur to me to email the endo, and I knew she was only in the office where we see her on Thursdays. Since Angelina started pumping on a Wednesday and that Thursday was okay and the following Thursday was her appointment I didn't see the point of calling the office. I think I learned my lesson though. But I also learned that the dr gave the pump trainer the okay to make adjustments because she joined us at Angelina's appointment. Things are so far, so good though. Fingers crossed.
One of the things that was the most frustrating is I just felt like we were on our own. I had gotten the impression that we were supposed to contact our pump trainer for adjustments but every time I reached out it seemed like she didn't return my calls, or if she did she didn't really DO anything. It didn't even occur to me to email the endo, and I knew she was only in the office where we see her on Thursdays. Since Angelina started pumping on a Wednesday and that Thursday was okay and the following Thursday was her appointment I didn't see the point of calling the office. I think I learned my lesson though. But I also learned that the dr gave the pump trainer the okay to make adjustments because she joined us at Angelina's appointment. Things are so far, so good though. Fingers crossed.
Related articles
- Insulin 101 - did I miss that class? (fifteenwaitfifteen.com)
- High/Low for Week of June 20, 2013 (chasinglows.wordpress.com)
- Untethered at the Beach (testguessandgo.com)
Thursday, July 25, 2013
Follow Me on Bloglovin'
Sunday, July 21, 2013
Angelina's Diabetes Summer 2014 Fundraiser
Wednesday, July 17, 2013
Pump Training
Thursday, July 11, 2013
High/Low Week of July 4, 2013
Related articles
- High/Low for Week of June 20, 2013 (chasinglows.wordpress.com)
- It's Here! (chasinglows.wordpress.com)
- High/Low Week of June 27, 2013 (chasinglows.wordpress.com)
Thursday, July 4, 2013
High/Low Week of June 27, 2013

 When I spoke with our rep on Tuesday she said she would be going over the contents of the box with us on Friday and discussing how to turn the pump on, etc. I just kind of laughed and told her I already had the whole thing set up and we've been using it, just without it being hooked up. Obviously there will still be a ton to learn, but most of what I have left to learn about it is going to be trial and error. Like knowing when it's time to change an infusion set if her numbers are higher than they should be. And, of course, learning how to do a site change. In theory I know how it works, and I've watched several Youtube videos, as well as the online training videos on the Medtronic website. In practice though, I haven't done it yet. Angelina won't let me put an infusion site on her until it's actually time to hook up. I asked if she wanted to do one on me, which she said no to. However, she said she would do one on Daddy. Daddy wasn't interested, lol.
So, the low for this week:
Monday David decided to stay home from work. The month of June is always super crazy busy at his work and he worked almost 3 weeks straight without a day off. Last week alone he worked 96 hours. He also came down with a cold last Friday so when Sunday was over (last day of the quarter) he told his supervisor he was taking sick time on Monday. We decided to go out for lunch and Angelina wanted pizza. If you're a t1 parent you know what pizza means. If you're not a t1 parent, let's just say that pizza is just one of those foods that T1 parents dread, lol. Pizza tends to have a pretty high carb count, but more than that it has a lot of fat in it so it tends to absorb more slowly and often ends with really high BG spikes a few hours after eating it. It's such a pain because it has an initial spike in BG, just like any carb containing food, but then it really spikes later. The later spike usually occurs after the fast-acting insulin has already peaked (which happens about 1 - 1 1/2 hours after taking it) meaning there isn't a ton of insulin working hard to counteract those carbs and it's more of a trickle after that 90 minute mark, while the pizza carbs tend to flood at about that time. So, when Angelina said she wasn't sure how many pieces of pizza she wanted and asked if she could take her insulin AFTER eating, I said fine. Her blood sugar was in range so I wasn't too worried about her getting too high before the insulin started working and I figured it could only be a good thing if it peaked a little later since I knew the pizza would.
Well, what happened is Angelina ate her pizza, I drew up her insulin and she refused to take it. This was after eating 80-100 carbs worth of pizza. She decided to crawl under the table and curl up in the corner on David's side of the booth. David decided that he wasn't going to play games with her and told her she was getting her shot whether she cooperated or not. Normally I would have tried to talk to her, maybe offer a bribe, but she just totally flipped out and started kicking and yelling and he was just done. D.O.N.E. So he caught her arm, held it as steady as possible and gave the injection. Then it was time to go and she wouldn't stop having her meltdown so he just picked her up and carried her out to the car. She was not happy, at all.
About halfway home he finally says "Angelina, Mom and I love you very much and we want you to be happy. We're not trying to control your life. We're trying to keep you ALIVE and healthy. Because if you don't take your insulin, you could die. And what kind of parents would we be if we just let you die because you were being stubborn and didn't want to let us take care of your health? This isn't a choice. You have to take insulin whether you like it or not. We don't like it either. And we don't like fighting with you about it. But we will do what we have to to make sure that you're safe and healthy. Because if we don't, you could die." Now, I know what you're thinking. That's a little harsh, she's only 9. I felt the same way. Until 2 minutes later when she said "You're right. You're just trying to take care of me because you love me."
I've read recently that this generation of kids with diabetes aren't likely to see long term complications and that it's unwise and unhelpful to tell them they'll have complications in their 60's if they dont' take care of their diabetes now. Because, seriously, I'm a lot closer to 60 than my kid is and I still do stupid stuff and don't take care of myself and that could have a negative impact on my health later, but right now I'm just living life. So, I can understand that a tween or teen is even less interested in what might happen when they're older. And talking about diabetic coma or death seems to be taking it a little far, but those are very real and could be very immediate consequences of not taking care of it. Or at the very least a hospital stay with DKA and just being very sick from that. Angelina's had enough hospital experiences to know she doesn't want more if it can be helped.
And then I read in the past few days about 2 seperate cases of parents being prosecuted for murder and neglect for not taking care of their kid's diabetes. In one case the parents refused to seek medical care for their child, who was obviously very sick, and opted instead to pray over their child, who eventually died. She was in DKA. She had never been diagnosed with T1, but that is what the diagnosis was after she died. Most parents would have taken their kid to the dr or the ER.
In the other case, a woman has been charged with gross negligence and her child is currently hospitalized and not expected to live. Apparently the child had known T1, but the mother wasn't giving insulin and hadn't checked the child's blood sugar for around a week prior to the child being taken to the hospital because someone else called 911. The article I read didn't have a ton of details as to why the mother wasn't giving the child insulin or checking their BG. It did state that the mother had asked for a ride to the pharmacy to pick up some insulin on the day that the roommate called 911 and the child was taken to the hospital. It's just so very sad.
I'm so afraid of someone trying to call child protective services on us because Angelina is causing a scene in a restaurant (this wasn't the first time, unfortunately.) and we end up having to restrain her to give her insulin. But then I read things like the above and I just feel like I would rather "get in trouble" for doing what needed to be done rather than my child getting sick and possibly dying because I did nothing. And isn't it messed up that I even have to worry about any of that? That if I provide medical care against her will I risk being accused of abuse, but if I don't I risk being accused of medical neglect? I just wish things could be simpler. I am hoping the pump helps.
When I spoke with our rep on Tuesday she said she would be going over the contents of the box with us on Friday and discussing how to turn the pump on, etc. I just kind of laughed and told her I already had the whole thing set up and we've been using it, just without it being hooked up. Obviously there will still be a ton to learn, but most of what I have left to learn about it is going to be trial and error. Like knowing when it's time to change an infusion set if her numbers are higher than they should be. And, of course, learning how to do a site change. In theory I know how it works, and I've watched several Youtube videos, as well as the online training videos on the Medtronic website. In practice though, I haven't done it yet. Angelina won't let me put an infusion site on her until it's actually time to hook up. I asked if she wanted to do one on me, which she said no to. However, she said she would do one on Daddy. Daddy wasn't interested, lol.
So, the low for this week:
Monday David decided to stay home from work. The month of June is always super crazy busy at his work and he worked almost 3 weeks straight without a day off. Last week alone he worked 96 hours. He also came down with a cold last Friday so when Sunday was over (last day of the quarter) he told his supervisor he was taking sick time on Monday. We decided to go out for lunch and Angelina wanted pizza. If you're a t1 parent you know what pizza means. If you're not a t1 parent, let's just say that pizza is just one of those foods that T1 parents dread, lol. Pizza tends to have a pretty high carb count, but more than that it has a lot of fat in it so it tends to absorb more slowly and often ends with really high BG spikes a few hours after eating it. It's such a pain because it has an initial spike in BG, just like any carb containing food, but then it really spikes later. The later spike usually occurs after the fast-acting insulin has already peaked (which happens about 1 - 1 1/2 hours after taking it) meaning there isn't a ton of insulin working hard to counteract those carbs and it's more of a trickle after that 90 minute mark, while the pizza carbs tend to flood at about that time. So, when Angelina said she wasn't sure how many pieces of pizza she wanted and asked if she could take her insulin AFTER eating, I said fine. Her blood sugar was in range so I wasn't too worried about her getting too high before the insulin started working and I figured it could only be a good thing if it peaked a little later since I knew the pizza would.
Well, what happened is Angelina ate her pizza, I drew up her insulin and she refused to take it. This was after eating 80-100 carbs worth of pizza. She decided to crawl under the table and curl up in the corner on David's side of the booth. David decided that he wasn't going to play games with her and told her she was getting her shot whether she cooperated or not. Normally I would have tried to talk to her, maybe offer a bribe, but she just totally flipped out and started kicking and yelling and he was just done. D.O.N.E. So he caught her arm, held it as steady as possible and gave the injection. Then it was time to go and she wouldn't stop having her meltdown so he just picked her up and carried her out to the car. She was not happy, at all.
About halfway home he finally says "Angelina, Mom and I love you very much and we want you to be happy. We're not trying to control your life. We're trying to keep you ALIVE and healthy. Because if you don't take your insulin, you could die. And what kind of parents would we be if we just let you die because you were being stubborn and didn't want to let us take care of your health? This isn't a choice. You have to take insulin whether you like it or not. We don't like it either. And we don't like fighting with you about it. But we will do what we have to to make sure that you're safe and healthy. Because if we don't, you could die." Now, I know what you're thinking. That's a little harsh, she's only 9. I felt the same way. Until 2 minutes later when she said "You're right. You're just trying to take care of me because you love me."
I've read recently that this generation of kids with diabetes aren't likely to see long term complications and that it's unwise and unhelpful to tell them they'll have complications in their 60's if they dont' take care of their diabetes now. Because, seriously, I'm a lot closer to 60 than my kid is and I still do stupid stuff and don't take care of myself and that could have a negative impact on my health later, but right now I'm just living life. So, I can understand that a tween or teen is even less interested in what might happen when they're older. And talking about diabetic coma or death seems to be taking it a little far, but those are very real and could be very immediate consequences of not taking care of it. Or at the very least a hospital stay with DKA and just being very sick from that. Angelina's had enough hospital experiences to know she doesn't want more if it can be helped.
And then I read in the past few days about 2 seperate cases of parents being prosecuted for murder and neglect for not taking care of their kid's diabetes. In one case the parents refused to seek medical care for their child, who was obviously very sick, and opted instead to pray over their child, who eventually died. She was in DKA. She had never been diagnosed with T1, but that is what the diagnosis was after she died. Most parents would have taken their kid to the dr or the ER.
In the other case, a woman has been charged with gross negligence and her child is currently hospitalized and not expected to live. Apparently the child had known T1, but the mother wasn't giving insulin and hadn't checked the child's blood sugar for around a week prior to the child being taken to the hospital because someone else called 911. The article I read didn't have a ton of details as to why the mother wasn't giving the child insulin or checking their BG. It did state that the mother had asked for a ride to the pharmacy to pick up some insulin on the day that the roommate called 911 and the child was taken to the hospital. It's just so very sad.
I'm so afraid of someone trying to call child protective services on us because Angelina is causing a scene in a restaurant (this wasn't the first time, unfortunately.) and we end up having to restrain her to give her insulin. But then I read things like the above and I just feel like I would rather "get in trouble" for doing what needed to be done rather than my child getting sick and possibly dying because I did nothing. And isn't it messed up that I even have to worry about any of that? That if I provide medical care against her will I risk being accused of abuse, but if I don't I risk being accused of medical neglect? I just wish things could be simpler. I am hoping the pump helps.
Related articles
- The thing about diabetes (diabetescounselling.com.au)
- The Truth About Glycemic Index (shaunballiah.wordpress.com)
- New Online Calculator for the Diabetes Math Impaired (diabetesmine.com)
- To Dose or not to Dose? (testguessandgo.com)
- Always is a Long Time (flowerdiabetes.wordpress.com)
